A chapter from HANDLING THE HARD QUESTIONS:
What Our Patients Are Asking Us About Rheumatic DiseaseRead and download this booklet on our Workforce Resource homepage
Each day, rheumatology nurses, nurse practitioners, and physician assistants field dozens of questions from their patients with rheumatic diseases, and they need to be able to properly and effectively communicate appropriate responses. This pocket guide includes a brief summary of evidence surrounding some of the most common—and challenging—questions that patients with rheumatoid arthritis, psoriatic arthritis, gout, and systemic lupus erythematosus are asking about. We hope you find this guide useful for your professional development and that it assists you with your day-to-day patient management.
Will I still be able to get pregnant despite having lupus?
Yes, with careful planning, treatment selection, and monitoring, a successful pregnancy is absolutely possible despite a diagnosis of lupus. The same holds true for other rheumatic diseases.
While autoimmune diseases can affect individuals of any age, newly-diagnosed SLE or another rheumatic disease can be particularly devastating to women of childbearing age. Some rheumatic diseases, including SLE, not only disproportionally affect women, but also tend to more commonly strike during childbearing years. Furthermore, rheumatic diseases by their very nature, as well as the medications used to manage them, can directly impact the timing of pregnancy planning as well as pregnancy outcomes.
Most rheumatic diseases have been associated with increased maternal and fetal complications compared with the general population. For instance, both SLE and RA have been associated with higher risks of Cesarean section delivery, preeclampsia, and preterm birth.1,2 Poorly controlled disease activity has been shown to increase the risk of adverse outcomes, whereas well controlled disease has been associated with improved outcomes.3
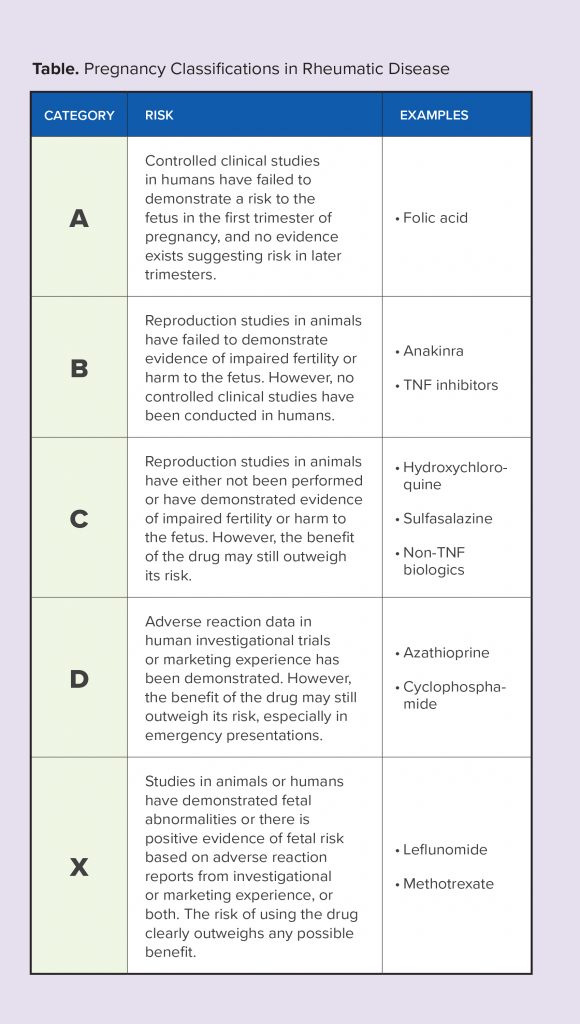
A number of the medications used to treat rheumatic diseases can be harmful to developing fetuses. Therefore, family planning counseling, including the use of contraceptives to prevent unintended pregnancies, is an integral part of providing comprehensive care.
When female patients diagnosed with a rheumatic disease are contemplating pregnancy or wish to conceive, disease activity should be well-controlled for at least 3-6 months prior to conception. During this time frame, therapies that have been determined to be unsafe for use throughout pregnancy, such as methotrexate, leflunomide, and non-TNF biologics (after 1st trimester), should be discontinued, with other pregnancy-compatible therapies started or adjusted to reach or maintain no/low disease activity. Therapy may also need to be adjusted during pregnancy in order to ensure safety of the mother and fetus during all trimesters. The choice of therapy during the postpartum period and beyond should focus on drugs that are safe for use during breastfeeding, when relevant.2-4
Disease-modifying therapies may also need to be adjusted or changed in male patients with a rheumatic disease interested in starting a family. For instance, it is recommended that methotrexate be discontinued 3 months prior to attempted conception in men due to the potential impact of the drug on sperm count.2
Undoubtedly, pregnancy planning and management in patients with a rheumatic disease is complex and requires a multidisciplinary care team approach. However, with careful planning, treatment selection, and monitoring, pregnancies can be successfully managed with the ultimate outcome—a healthy baby—as the result.
References
1. Nuki G, Doherty M, Richette P. Current management of Arkema EV, Palmsten K, Sjowall C, Svenungsson E, Salmon JE, Simard JF. What to expect when expecting with systemic lupus erythematosus (SLE): A population-based study of maternal and fetal outcomes in SLE and pre-SLE. Arthritis Care Res Hoboken). 2016;68(7):988‑994.
2. Krause ML, Makol A. Management of rheumatoid arthritis during pregnancy: challenges and solutions. Open Access Rheumatol. 2016;8:23-36.
3. Birru Talabi M, Clowse MEB, Schwarz EB, Callegari LS, Moreland L, Borrero S. Family planning counseling for women with rheumatic diseases. Arthritis Care Res (Hoboken). 2018;70(2):169-174.
4. Flint J, Panchal S, Hurrell A, et al. BSR and BHPR guideline on prescribing drugs in pregnancy and breastfeeding-Part I: standard and biologic disease modifying anti-rheumatic drugs and corticosteroids. Rheumatology (Oxford). 2016;55(9):1693-1697.