A chapter from HANDLING THE HARD QUESTIONS:
What Our Patients Are Asking Us About Rheumatic DiseaseRead and download this booklet on our Workforce Resource homepage
Each day, rheumatology nurses, nurse practitioners, and physician assistants field dozens of questions from their patients with rheumatic diseases, and they need to be able to properly and effectively communicate appropriate responses. This pocket guide includes a brief summary of evidence surrounding some of the most common—and challenging—questions that patients with rheumatoid arthritis, psoriatic arthritis, gout, and systemic lupus erythematosus are asking about. We hope you find this guide useful for your professional development and that it assists you with your day-to-day patient management.
Does a diagnosis of Rheumatoid Arthritis (RA) mean I am going to eventually be crippled or disabled?
Not anymore.
RA is considered a chronic disease. Decades ago, many patients with poorly controlled or untreated RA developed bony joint deformities and progressive and irreversible damage in multiple joints, such as the hands, wrists, feet, spine, shoulder, hips, and knees.1 These sorts of changes often contributed to reduced functional status and the ability to physically perform activities of daily living without limitations. By the end of their lives, some patients with RA were confined to a wheelchair and had significantly deformed hands and wrists.2
Fortunately, over the last several decades, significantly more effective medications and treatment strategies have become available, and outcomes for patients with RA have substantially improved.3
Given the impact of RA on functional, radiologic, and structural outcomes, early and intensive treatment with disease modifying anti-rheumatic drugs (DMARDs) is now considered best practice.4 RA treatment guidelines recommend using a treat-to-target strategy, in which patient response to DMARD therapy is closely monitored every 1-3 months and therapies are adjusted in response to disease activity. The goal of this approach is to rapidly reach a state of sustained remission or low disease activity.5,6
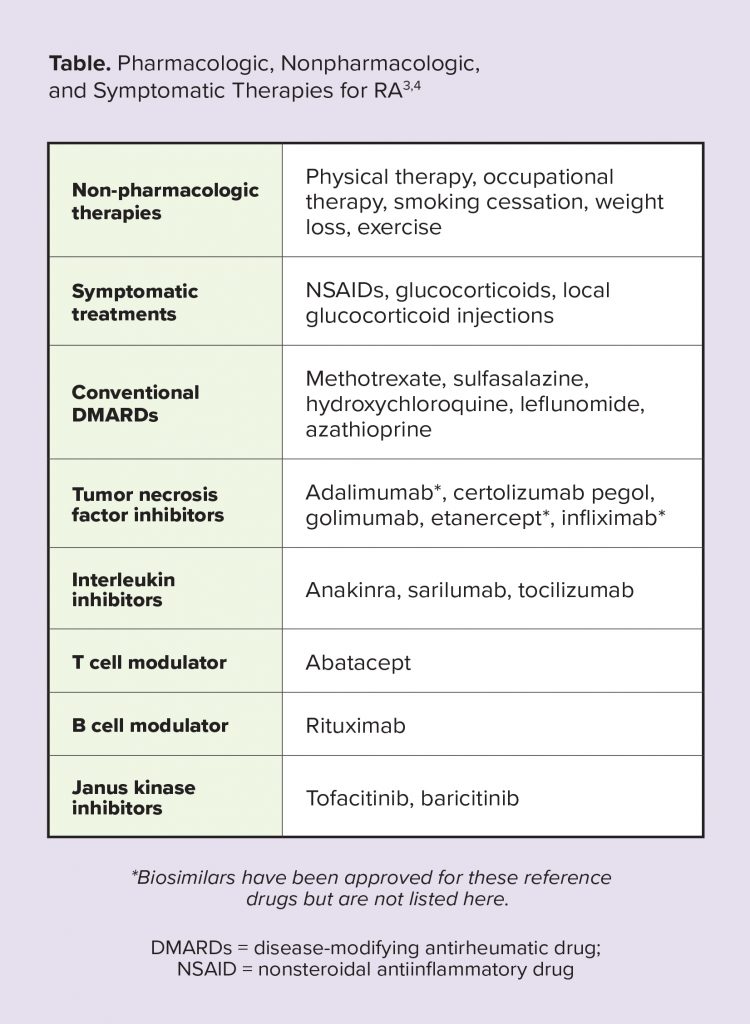
Patients who receive DMARD therapy earlier in the disease course (ideally, less than 3 to 6 months after symptom onset) experience greater improvements in functional status over both the short- and longterm compared with those with a longer duration of symptoms prior to starting therapy.4 Similarly, the treat-to-target approach has been associated with improvements in outcomes, such as decreased disease activity, reduced joint damage progression, increased functional ability, and improved quality of life.7,8
References
1. Hochberg M, et al. Clinical features of rheumatoid arthritis. In: Rheumatology. 6th ed. Philadelphia, PA: Mosby Elsevier; 2015.
2. Norton S, Sacker A, Dixey J, et al. Trajectories of functional limitation in early rheumatoid arthritis and their association with mortality. Rheumatology (Oxford). 2013;52(11):2016-2024.
3. Kievit W, Fransen J, de Waal Malefijt MC, den Broeder AA, van Riel PL. Treatment changes and improved outcomes in RA: an overview of a large inception cohort from 1989 to 2009. Rheumatology (Oxford). 2013;52(8):1500-1508.
4. Monti S, Montecucco C, Bugatti S, Caporali R. Rheumatoid arthritis treatment: the earlier the better to prevent joint damage. RMD Open. 2015;1(Suppl1):e000057.
5. Smolen JS, Landewe R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76(6):960-977.
6. Singh JA, Saag KG, Bridges SL, Jr., et al. 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2016;68(1):1-25.
7. Sakellariou G, Scire CA, Verstappen SM, Montecucco C, Caporali R. In patients with early rheumatoid arthritis, the new ACR/EULAR definition of remission identifies patients with persistent absence of functional disability and suppression of ultrasonographic synovitis. Ann Rheum Dis. 2013;72(2):245-249.
8. Pincu T, Castrejon I. Evidence that the strategy is more important than the agent to treat rheumatoid arthritis. Bull Hosp Jt Dis. 2013;71(71):8.