A chapter from HANDLING THE HARD QUESTIONS:
What Our Patients Are Asking Us About Rheumatic DiseaseRead and download this booklet on our Workforce Resource homepage
Each day, rheumatology nurses, nurse practitioners, and physician assistants field dozens of questions from their patients with rheumatic diseases, and they need to be able to properly and effectively communicate appropriate responses. This pocket guide includes a brief summary of evidence surrounding some of the most common—and challenging—questions that patients with rheumatoid arthritis, psoriatic arthritis, gout, and systemic lupus erythematosus are asking about. We hope you find this guide useful for your professional development and that it assists you with your day-to-day patient management.
Why do I often feel worse right after starting a new medication? | Gout
Initial worsening of symptoms is not uncommon in gout patients starting on a new medication, but importantly is not an indicator that their medication is not working.
Medications are a key component of gout management and are used for both the treatment of acute attacks as well as to prevent future attacks.
The first goal when treating gout is to address the acute attack, with medications used as soon as possible to reduce inflammation and control symptoms. Medications may typically include non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, intra-articular injections of corticosteroids, and/ or colchicine.1
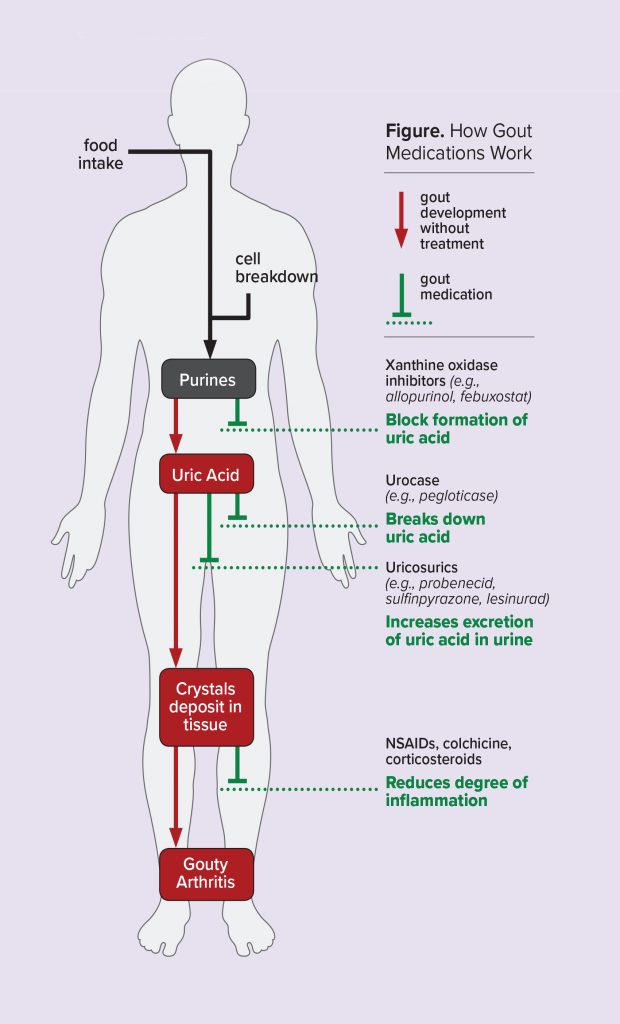
The second goal of gout management is to reduce or prevent future acute attacks. As hyperuricemia is a key component in the development of gout, urate lowering therapy (ULT) is recommended for most patients. This is done to achieve serum uric acid levels below saturation thresholds, promote crystal dissolution, and prevent future crystal formation and attacks.1,2 A number of different drugs are available to reduce uric acid levels, either through reducing the formation of uric acid, increasing the breakdown of uric acid, or increasing the renal excretion of uric acid.3
As an acute attack resolves and patients begin ULT, urate crystals that were deposited throughout the body may begin to disperse. While the risk of gout attacks is reduced after approximately 1 year of ULT treatment, ULT does not reduce the risk during the first 6 months. As such, patients may experience a spike in acute flares, which can lead to reduced patient adherence to treatment as they feel their medication might not be working. As such, prophylaxis, typically with colchicine or NSAIDs, is usually used during the first 6 months of ULT to prevent acute flares.1,2
References
1. Nuki G, Doherty M, Richette P. Current management of gout: practical messages from 2016 EULAR guidelines. Pol Arch Intern Med. 2017;127(4):267-277.
2. Qaseem A, Harris RP, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Management of acute and recurrent gout: A clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(1):58-68. RNS Professional Education: Rheumatic Disease 29
3. Guttmann A, Krasnokutsky S, Pillinger MH, Berhanu A. Pegloticase in gout treatment – safety issues, latest evidence and clinical considerations. Ther Adv Drug Saf. 2017;8(12):379-388.