A chapter from HANDLING THE HARD QUESTIONS:
What Our Patients Are Asking Us About Rheumatic DiseaseRead and download this booklet on our Workforce Resource homepage
Each day, rheumatology nurses, nurse practitioners, and physician assistants field dozens of questions from their patients with rheumatic diseases, and they need to be able to properly and effectively communicate appropriate responses. This pocket guide includes a brief summary of evidence surrounding some of the most common—and challenging—questions that patients with rheumatoid arthritis, psoriatic arthritis, gout, and systemic lupus erythematosus are asking about. We hope you find this guide useful for your professional development and that it assists you with your day-to-day patient management.
Will my disease ever go away? | Psoriatic Arthritis (PsA)
Unfortunately, the answer is likely no.
PsA is a heterogenous disease in both presentation and disease course. As such, for some patients, the clinical course of the disease may follow a waxing and waning course, characterized by a series of remissions and flares. Fewer than 20% of individuals with PsA will experience prolonged remission.
Of individuals who develop PsA, an estimated 25-30% will experience relatively mild joint inflammation over time, associated with only limited disability. In contrast, without recommended treatment, up to 60% of affected patients will experience progressive and destructive arthritis.1 PsA is associated with negative impacts on health related quality of life as well as higher health costs and utilization.
Similar to other forms of autoimmune arthritis, such as RA, higher levels of disease activity are associated with more progressive joint damage. As such, early identification and initiation of treatment is key to improving long-term outcomes.2
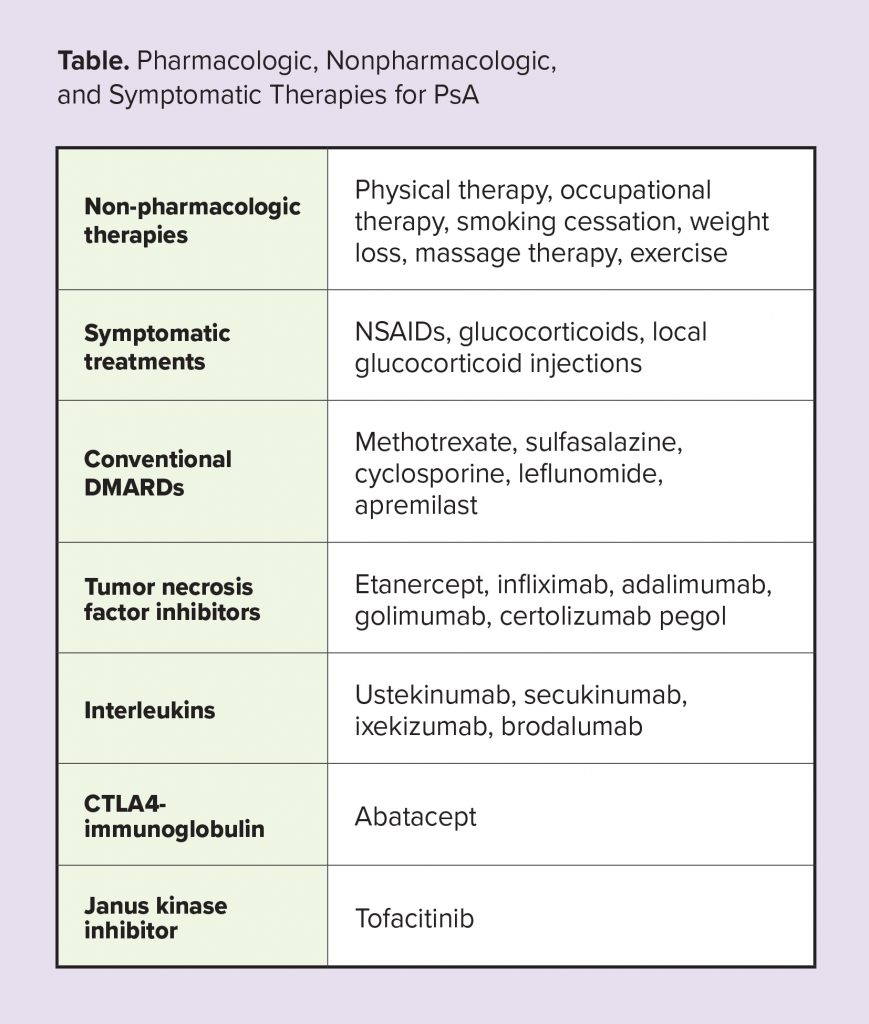
Both non-pharmacologic and pharmacologic approaches to the treatment of PsA can reduce inflammation, ameliorate symptoms, and, in some cases, even result in remission. Given the autoimmune underpinnings of PsA, disease-modifying drugs are typically used in patients with active disease to address the underlying disease process.2 Similar to treatment approaches for other chronic diseases, a treat-to-target approach to the management of PsA has been associated with improved outcomes.3
One study found that 58% of patients with PsA were able to achieve remission, as measured by disease activity score, after one year of treatment with TNF inhibitor therapy.4 However, while some patients may reach a state of low disease activity or remission with treatment, evidence indicates that most patients (~75%) experience a recurrence or flare within several months after stopping medication.5 So, while medications may “quiet” the disease activity, they do not cure PsA, and long-term drug-free remission is likely unattainable. In that sense then, the disease will never “go away.”
References
1. Menter A. Psoriasis and psoriatic arthritis overview. Am J Manag Care. 2016;22(8 Suppl):s216-224.
2. Singh JA, Guyatt G, Ogdie A, et al. Special Article: 2018 American College of Rheumatology/National Psoriasis Foundation guideline for the treatment of psoriatic arthritis. Arthritis Rheumatol. 2019;71(1):5-32.
3. Tucker LJ, Ye W, Coates LC. Novel concepts in psoriatic arthritis management: Can we treat to target? Curr Rheumatol Rep. 2018;20:9.
4. Saber TP, Ng CT, Renard G, et al. Remission in psoriatic arthritis: is it possible and how can it be predicted? Arthritis Res Ther. 2010;12(3):R94.
5. Araujo EG, Finzel S, Englbrecht M, et al. High incidence of disease recurrence after discontinuation of diseasemodifying antirheumatic drug treatment in patients with psoriatic arthritis in remission. Ann Rheum Dis. 2015;74(4):655-660