A chapter from HANDLING THE HARD QUESTIONS:
What Our Patients Are Asking Us About Rheumatic DiseaseRead and download this booklet on our Workforce Resource homepage
How did I get rheumatoid arthritis?
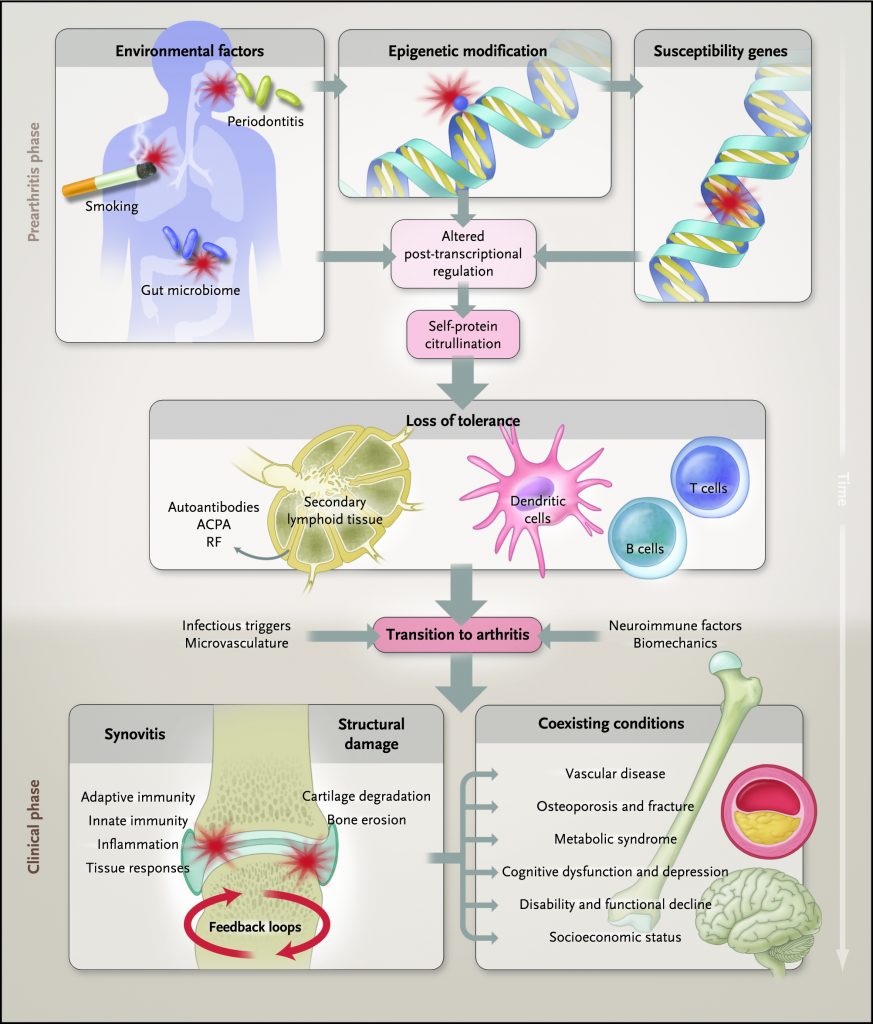
There are a variety of factors that may have contributed to your developing rheumatoid arthritis (RA), a chronic, autoimmune disease. In the average individual, the immune system protects the body from disease and foreign substances such as bacteria and viruses through a complex interplay of different cells involved in the immune response.1
The ability of the immune system to recognize “self” from “non-self” is key to a properly functioning immune system. However, in individuals with autoimmune conditions such as RA, something in the immune system goes awry. The immune system loses its ability to recognize and tolerate the body as “self.” As a result, the immune system mistakenly starts attacking the body’s own cells and healthy tissue.1
In individuals diagnosed with RA, the immune cells often target the lining of the joints, called the synovium. The damage caused by this process leads to inflammation and, eventually, cartilage and bone destruction. While many people think of RA as just a joint disease, it can also affect other tissues and systems in the body, such as the cardiovascular and pulmonary systems. This system-wide, dysfunctional immune response explains why individuals with RA may experience symptoms such as fatigue, fever, and/or weight loss in addition to red, swollen, and painful joints.1
The definitive cause of RA is still unknown; however, it is widely believed to be due to a combination of susceptibility genes, environmental factors, and chance.1
More than 100 genes have been associated with an increased susceptibility for developing RA or influencing the degree of disease severity.2 However, not everyone with an RA susceptibility gene develops RA, suggesting other factors are involved. It is generally accepted that an environmental event of some sort is required to trigger the loss of “self” tolerance and development of RA. Examples of environmental factors associated with the development of RA include smoking, periodontal disease, altered gastrointestinal and respiratory microbiome, and certain infections.1
Furthermore, females are 2-3 times more likely to develop RA than males. While reasons for this are not yet fully understood, it is thought to be due to the effects of some hormones (e.g., estrogen and prolactin, which are both considered proinflammatory hormones) as well as neuroimmunological interactions.1,3
References
1. McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Eng J Med. 2011;365(23):2205-2219.
2. Firestein GS, McInnes IB. Immunopathogenesis of rheumatoid arthritis. Immunity. 2017;46(2):183‑196.
3. Oliver JE, Silman AJ. Why are women predisposed to autoimmune rheumatic diseases? Arthritis Res Ther. 2009;11(5):252.